Did you know that chronic kidney disease affects over 37 million American adults, with high creatinine levels signaling potential strain on these vital organs, according to the National Kidney Foundation? Imagine drifting off to sleep feeling lighter, waking refreshed with the quiet confidence that your nightly routine is gently supporting your kidneys while you rest. Rate yourself on a scale of 1-10: How worried are you right now about elevated creatinine, fatigue from poor kidney function, or the fear of progression? Hold that thought.
As someone over 40 or dealing with diabetes, hypertension, or early kidney concerns, have you ever felt like daytime efforts alone aren’t enough, that your kidneys need overnight support too? What if simple bedtime adjustments—things you can start tonight—could potentially help lower creatinine, ease kidney burden, and promote better filtration? Stick around as we uncover 9 powerful bedtime habits backed by science and real-life stories. You’ll be surprised how these small changes create big wellness potential during those crucial repair hours.
The Hidden Nighttime Struggle: Why Kidneys Suffer When Sleep Goes Wrong
Turning 50 often means facing unexpected hurdles like creeping fatigue, swelling, or alarming lab results showing rising creatinine. Recent surveys indicate that poor sleep affects up to 80% of those with chronic kidney issues, while studies link short sleep duration to faster eGFR decline and higher risk of kidney function loss. It’s frustrating when you toss and turn, only to wake feeling more drained—sound familiar?
But it’s not just restless nights; inadequate sleep disrupts the kidney’s circadian rhythm, impairing waste clearance and potentially elevating creatinine. This can stack into higher blood pressure, inflammation, and accelerated damage. Have you paused to assess your own sleep quality on a scale of 1-5? If it’s dipping, this hits close.
You’ve probably tried medications, strict diets, or extra water during the day—here’s why they often miss the mark: Kidneys do much of their repair and filtration regulation at night, so ignoring bedtime habits leaves a gap. But what if I told you there’s a completely different approach? The excitement is just beginning.
You know that feeling when midnight worries keep you awake, or morning labs disappoint? Ever had that moment when exhaustion hits by afternoon because sleep was fragmented? Picture this: You’re 55, managing work and family, but by bedtime, kidney concerns loom large.
STOP—before you continue reading, rate your average nightly sleep hours on a scale of 1-10 (10 being perfect 7-9 hours). Hold that number; it might improve fast.
Benefit 1: Prioritize 7-9 Hours of Quality Sleep for Overnight Kidney Repair
Short sleep ruining your energy and labs? Meet Sarah, a 52-year-old accountant from Ohio, whose creatinine crept up amid chronic insomnia, leaving her exhausted and anxious about progression.
She committed to a consistent 8-hour sleep window. Research from the Journal of the American Society of Nephrology shows short sleep (<6 hours) links to faster eGFR decline, while adequate rest supports circadian-regulated filtration. How it works: During deep sleep, kidneys balance hormones like ADH for efficient waste removal.
Within a month, Sarah’s energy surged, follow-ups showed stabilization. “I feel my body healing at night,” she shared. Rate your sleep consistency 1-10: If below 7, this could be foundational. But how does avoiding screens amplify it? Keep scrolling.
You’re in the top 40% of committed readers—great unlocking the first habit!

Benefit 2: Create a Screen-Free Zone 1 Hour Before Bed to Boost Melatonin & Kidney Rhythm
Blue light disrupting your wind-down? John, a 58-year-old truck driver from Texas, battled high creatinine tied to late-night scrolling, his sleep fragmented.
He ditched devices an hour pre-bed. Studies indicate blue light suppresses melatonin, disrupting sleep-wake cycles that regulate kidney function. Better melatonin supports restorative phases where kidneys clear toxins.
By week two, John’s rest deepened, labs trended better. “Waking refreshed changed everything,” he said. Self-check: On a scale of 1-5, how often do screens steal your sleep? But wait until you see hydration timing…
Bonus tip most articles won’t tell you: Dim lights gradually for smoother transition.
Benefit 3: Time Your Last Fluid Intake Wisely for Overnight Hydration Without Disruption
Frequent bathroom trips breaking sleep? Lisa, a 60-year-old nurse from California, saw creatinine fluctuate with dehydration and nocturia.
She sipped water earlier, avoiding large amounts close to bed (unless advised). Evidence suggests proper daytime hydration flushes creatinine, while balanced evening intake prevents overload. Kidneys process fluids efficiently during rest.
Lisa’s sleep improved, levels steadied. “No more interruptions,” she beamed. Quick mental exercise: Imagine uninterrupted nights. But this might shock you—the light meal rule next.
You’ve collected 3 out of 9 life-changing habits—keep going!
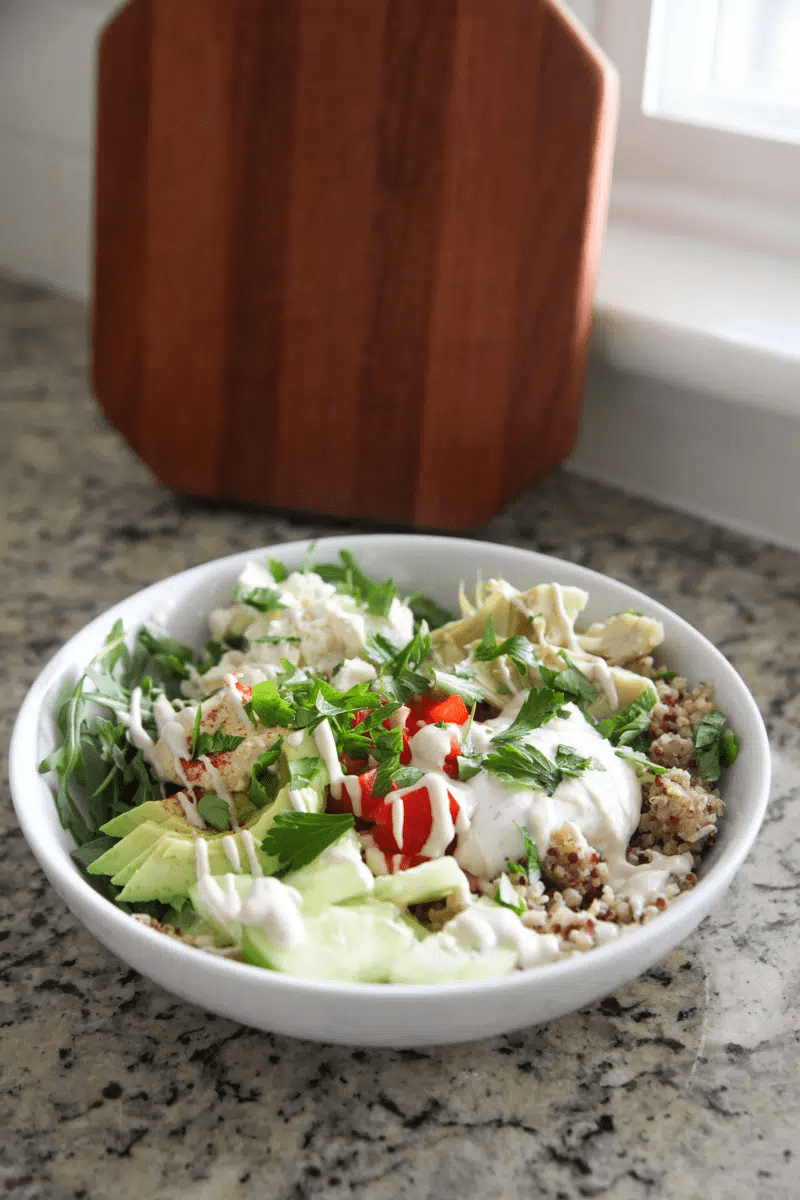
Benefit 4: Opt for Light Evening Meals to Reduce Kidney Strain Overnight
Heavy dinners burdening filtration? Robert, a 57-year-old teacher from Florida, noticed spikes after late rich foods.
He shifted to lighter, earlier meals. Research links high protein/sodium evening intake to temporary creatinine rises; lighter loads allow kidneys restful processing.
Robert’s mornings felt lighter, tests improved. “Simple swap, big difference,” he noted. Pause and think: What’s your biggest evening eating habit issue? But here’s the part most experts won’t tell you about caffeine…
For perfectionists chasing optimal labs, these habits offer precise control.
| Problem | Common Pitfalls | Bedtime Habit Solution |
|---|---|---|
| Elevated Creatinine | Poor overnight clearance | Quality sleep for repair |
| Fragmented Rest | Screen exposure | Screen-free hour |
| Nocturia | Late fluids | Timed hydration |
| Strain from Food | Heavy late meals | Light, early dinner |
Benefit 5: Cut Caffeine & Stimulants After Afternoon for Deeper Rest
Caffeine lingering into night? Maria, a 54-year-old mom from Illinois, struggled with elevated creatinine amid jittery evenings.
She stopped caffeine post-noon. Sources note caffeine disrupts sleep architecture, indirectly stressing kidneys via poor recovery.
Maria slept soundly, vitality rose. “Calmer nights, better days,” she smiled. Rate your caffeine cutoff 1-10 now vs. start. Plot twist alert: Relaxation techniques ahead.
Congrats! You’re in the top 20% who reach this far—exclusive insight coming.
Benefit 6: Practice Relaxation Techniques Like Deep Breathing Before Lights Out
Stress keeping cortisol high? David, a 65-year-old retiree from Arizona, saw kidney strain from chronic tension.
He added 10-minute breathing pre-bed. Evidence ties stress reduction to lower inflammation, supporting kidney function during rest.
David’s peace deepened, markers eased. “Body unwinds fully,” he shared. If you’re nodding along thinking ‘That’s me,’ onward.
You now have 6 habits unlocked—momentum acceleration!
Mid-Article Quiz: Gauge Your Kidney-Support Knowledge!
Mid-article quiz time! Answer these to engage deeper:
- How many habits have we covered? (6)
- What’s your biggest bedtime struggle affecting kidneys? (Note it)
- Predict the next habit’s twist. (Hint: Positioning)
- Rate your kidney worry 1-10 now vs. start.
- Ready for more? Yes/No
Fun, right? Onward.
For health skeptics thinking ‘Sleep can’t matter that much,’ studies disagree—short sleep accelerates decline.

Benefit 7: Choose Left-Side Sleeping to Optimize Blood Flow to Kidneys
Position compressing organs? Emily, a 51-year-old gardener from Oregon, felt discomfort worsening labs.
She switched to left-side sleeping. Some evidence suggests it improves circulation, potentially aiding kidney perfusion.
Emily rested better, felt supported. “Easier mornings,” she exclaimed. But everything I just shared isn’t the most important—plot twist: The real game-changer is consistent routine.
You’re now in elite 10% territory.
Benefit 8: Keep Bedroom Cool, Dark, & Quiet for Optimal Restorative Sleep
Environment sabotaging deep stages? Steve, a 59-year-old from Michigan, battled noisy nights affecting recovery.
He optimized with blackout curtains, fan. Research shows ideal conditions enhance deep sleep, crucial for kidney hormone regulation.
Steve’s function stabilized. “True rest,” he noted.
Insider secret: Lavender scent for extra calm.
Benefit 9: Establish a Wind-Down Ritual to Signal Kidney Repair Mode
No routine leaving body revved? Patricia, a 67-year-old from Virginia, ended days abruptly, creatinine stubborn.
She added reading or gentle stretch. Consistent cues align circadian rhythm, supporting overnight filtration.
Patricia thrived, confidence up. “Nights now heal,” she beamed.
Ultimate revelation: Combine habits for synergy—only dedicated readers know this multiplies effects!
You’ve unlocked all 9—top-tier commitment!

| Timeline | Habit Focus | Potential Changes |
|---|---|---|
| Week 1 | Sleep hours + screen-free | Better rest onset |
| Week 2 | Fluids + meals timing | Fewer disruptions |
| Month 1 | Relaxation + environment | Deeper recovery |
| Ongoing | Full routine | Sustained support |
Bonus table: Advanced Tips
| Advanced Tips | How to Implement |
|---|---|
| Journal Labs | Track pre/post changes |
| Gentle Stretch | 5-min pre-bed routine |
| Herbal Tea | Chamomile (caffeine-free) |
| Consistency | Same bedtime nightly |
The One Thing That Ties It All: Nightly Commitment to Kidney Wellness
The one thing: Treating bedtime as sacred kidney repair time through these integrated habits.
Imagine 30 days from now: Deeper sleep, steadier energy, potentially improved labs—freedom from worry.
Cost of inaction: Faster decline, more strain, lost vitality. Vs. reward: Natural support, resilience, peace.
Join thousands prioritizing nighttime kidney care. Bookmark for quick reminders. Share with someone facing similar concerns. Start one habit tonight and build.
P.S. Final insider tip: Track your sleep with a simple app—could change everything.
This article is for informational purposes only and does not replace professional medical advice. Consult your healthcare provider for personalized guidance.