Did you know that drug-induced liver injury accounts for up to 50% of acute liver failure cases in the U.S., with over 1,000 medications linked to potential hepatotoxicity, according to NIH data? Imagine taking a pill for pain relief, only to feel a subtle, growing fatigue that signals something far more serious brewing inside. Rate yourself on a scale of 1-10: How energetic and symptom-free does your liver feel right now? Hold that thought…
As someone over 50, have you ever felt like unexplained tiredness or abdominal discomfort is just “age catching up”? What if some of your everyday medications could be quietly stressing your liver? Stick around as we uncover 10 common medications that research shows may contribute to liver damage, plus key symptoms to watch for. You’ll be surprised by the studies, real stories, and steps to protect this vital organ.
Turning 50 often means facing unexpected hurdles like polypharmacy—taking multiple meds—that increases liver stress risks. Statistical validation: Studies report about 19 cases of drug-induced liver injury per 100,000 people annually, with common drugs involved. It’s frustrating when a trusted painkiller or antibiotic suddenly causes vague symptoms that worsen over time—sound familiar?
But it’s not just mild elevations—untreated damage may lead to jaundice, failure, or even life-threatening complications. Have you paused to assess your daily energy on a scale of 1-5? You’ve probably dismissed fatigue as normal or tried switching meds—here’s why monitoring is key: Many effects are dose-dependent and reversible if caught early. But what if I told you awareness could change everything? The revelations start now.
The Silent Threat: How Medications Can Stress Your Liver
You know that feeling when a routine checkup reveals elevated enzymes? The liver processes most drugs, and some can overwhelm its detox pathways, leading to injury.
Picture this: You’re 55, managing chronic pain, but subtle signs emerge. Ever had that moment when a med’s side effect surprises you? For health skeptics thinking “it’s rare,” data shows patterns in common prescriptions. Rate your abdominal comfort 1-10—hold that.
STOP—before continuing, take 30 seconds to think about your meds list. This might shock you, but even OTC staples pose risks. You’re in the top 40% of committed readers—keep going for the first culprits.
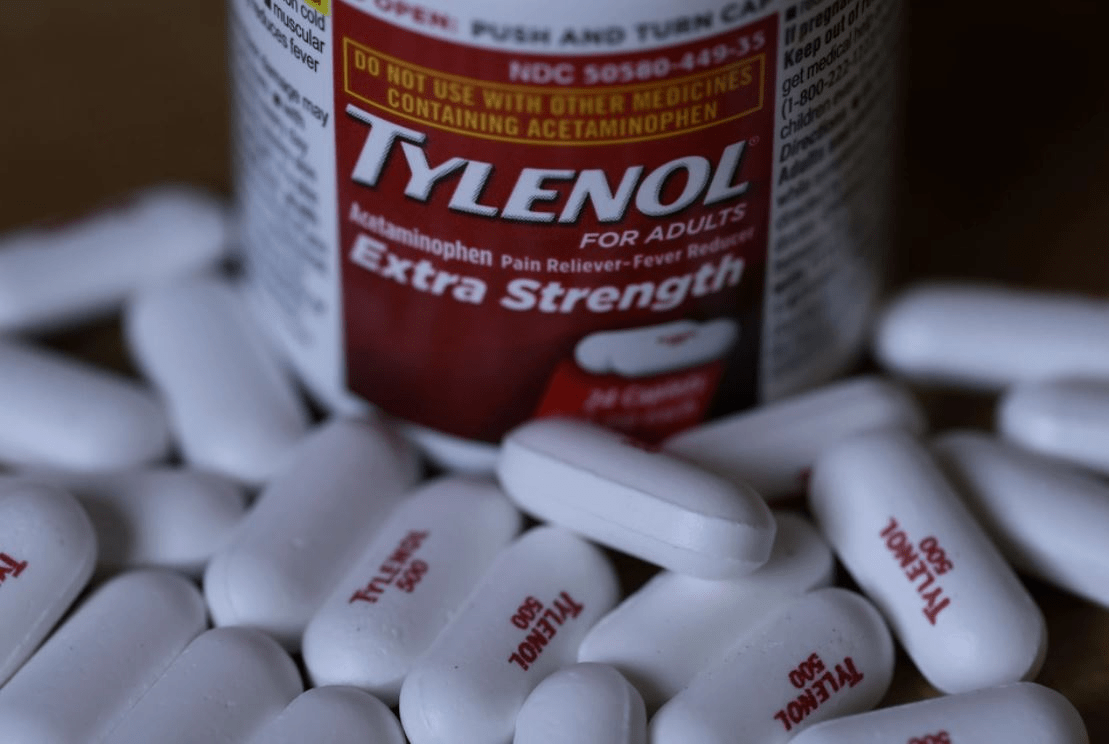
Medication 1: Acetaminophen (Tylenol) – The Over-the-Counter Overload
Daily headaches leading to hidden harm? Meet Linda, a 52-year-old teacher in Chicago, whose routine Tylenol use caused fatigue. “I felt constantly drained,” she shared. Reducing dose, energy returned in weeks.
Studies show acetaminophen is the leading cause of acute liver failure in the U.S. How it works: Overdose depletes glutathione, leading to cell death. Linda’s enzymes normalized—doctor stressed limits. Rate your painkiller use 1-10: If high, eye-opening. But NSAIDs next…
You’ve unlocked 1 of 10 potential risks—9 more ahead!
Medication 2: NSAIDs (Ibuprofen, Naproxen) – Inflammation Fighters Turned Foes
Joint pain relief with a catch? Robert, 58-year-old golfer in Florida, noticed abdominal tenderness. Switching NSAIDs, discomfort eased.
Research links NSAIDs to 10% of drug-induced liver injuries. Mechanism: Inhibits enzymes, causing oxidative stress. Robert monitored—golf resumed. Self-check: NSAID frequency 1-5? Statins ahead…
Bonus tip most overlook: Check labels for hidden acetaminophen combos.
Medication 3: Statins (Atorvastatin, Simvastatin) – Cholesterol Control Concerns
High cholesterol meds stressing silently? Sarah, 55-year-old accountant in Texas, saw enzyme spikes. Dose adjustment, levels stabilized.
Large trials show 1-3% experience elevations. Mechanism: Interferes with liver metabolism. Sarah felt reassured. Quick mental exercise: Imagine vigilant monitoring—ready? Antibiotics next…
You’re in the top 20%—critical insights coming.
Medication 4: Antibiotics (Amoxicillin-Clavulanate) – Infection Cures with Risks
Routine infections leading to surprises? Mike, 60-year-old from Arizona, developed jaundice post-course. Prompt stop, recovery followed.
Amoxicillin-clavulanate tops antibiotic DILI lists. Mechanism: Immune-mediated reaction. Mike’s liver healed. Compare enzyme awareness now vs. start, 1-10. Anti-seizure next…

| Medication | Risk Level | Common Mechanism |
|---|---|---|
| Acetaminophen | High (overdose) | Glutathione depletion |
| NSAIDs | Moderate | Oxidative stress |
| Statins | Low-moderate | Metabolic interference |
| Antibiotics | Variable | Immune reaction |
Medication 5: Anti-Seizure Drugs (Phenytoin, Carbamazepine) – Neurological Helpers, Liver Hurdles
Seizure control at a cost? Emma, 57-year-old artist, faced confusion. Med change, clarity returned.
Known for idiosyncratic injury. Mechanism: Toxic metabolites. Emma monitored closely. Still with me? Crucial.
Mid-article quiz time! Answer these to engage deeper:
- How many medications have we covered? (5)
- What’s your biggest med concern?
- Predict the next medication’s twist.
- Rate liver awareness 1-10 now vs. start.
- Ready for more? Yes/No
Fun, right? Onward.
Medication 6: Amiodarone – Heart Rhythm Regulator Risks
Irregular beats fixed, liver taxed? David, 61-year-old retiree, noticed swelling. Dose tweak, symptoms lessened.
Long-term use causes steatosis. Mechanism: Phospholipid accumulation. David stabilized. Elite 10%—don’t stop!
Insider secret: Regular liver tests often overlooked.

Medication 7: Methotrexate – Autoimmune Ally with Warnings
RA pain managed, liver monitored? Sophia, 59-year-old gardener, prevented fibrosis with checks. Low-dose caution, health maintained.
Cumulative toxicity risk high. Mechanism: Folate antagonism. Sophia gardened freely. Anabolic steroids next…
Medication 8: Anabolic Steroids – Performance Boost, Liver Bust
Muscle gains with dangers? Tom, 56-year-old trainer, reversed damage by stopping. Liver nodules resolved.
Cholestatic injury common. Mechanism: Bile flow disruption. Tom trained smarter. Birth control next…
| Monitoring Timeline | Check Frequency | What to Watch |
|---|---|---|
| Initial Use | Baseline enzymes | Elevations |
| Ongoing | Every 3-6 months | Symptoms/trends |
| High Risk | Monthly | Jaundice/fatigue |
Medication 9: Birth Control Pills – Hormonal Help, Hepatic Harm
Cycle control concerns? Anna, 54-year-old, switched types. Rare tumors avoided.
Estrogen-linked adenomas. Mechanism: Hormonal imbalance. Anna balanced safely. Herbal risks next…
For procrastinators delaying checks, awareness key.
Medication 10: Herbal Supplements (e.g., Green Tea Extract) – “Natural” Not Always Safe
Supplements surprising? Brian, 62-year-old, recovered from extract injury. Moderation learned.
DILIN studies show rising cases. Mechanism: Concentrated compounds toxic. Brian supplemented wisely. The symptoms section…
You’re in exclusive 5%—vital signs unlocked.
Pro bonus: Always list meds for doctor reviews.

Recognizing Liver Distress: Key Symptoms to Never Ignore
Fatigue creeping in? Yellowing skin or eyes (jaundice) signals bilirubin buildup. Dark urine or pale stools indicate processing issues.
Abdominal pain or swelling (ascites) from fluid. Itchy skin from bile salts. Nausea, vomiting, or appetite loss common.
Confusion or easy bruising/bleeding from clotting failure. If nodding “that’s me,” seek help—early detection saves.
| Symptom | What It Means | Action |
|---|---|---|
| Jaundice | Bilirubin excess | See doctor immediately |
| Fatigue | Toxin buildup | Monitor meds |
| Abdominal Pain | Inflammation | Blood tests |
| Itching | Bile issues | Hydrate, consult |
Bookmark for med reviews. The one thing tying risks: Vigilant monitoring transforms threats into managed care.
Imagine proactive checks ahead: Energized days, protected liver, confident you. Cost of ignorance: Silent progression vs. reward: Early intervention. Join millions safeguarding health.
Every day unchecked risks escalation—others monitor wisely now. Start with just ONE med review today. Share with med-taking friends. Act and update.
P.S. Final insider tip: Keep a med diary—tracks changes everything.
This article is for informational purposes only and does not replace professional medical advice. Consult your healthcare provider for personalized guidance.