Did you know that about 13,000 new cases of cervical cancer are diagnosed in the United States each year, with around 4,000 women losing their lives to this preventable disease—yet early detection dramatically improves outcomes?
Imagine noticing a subtle change—like unexpected spotting or unusual discharge—and realizing it could be your body’s quiet alert to something serious, potentially catching it before it advances.
Rate yourself on a scale of 1-10: How confident are you that you’d recognize an unusual symptom in your reproductive health right now? Hold that number—we’re about to sharpen your awareness.
As someone in your 30s, 40s, or beyond managing work, family, and self-care, have you ever brushed off irregular bleeding or pelvic discomfort as “just hormones” or stress?
What if paying attention to these often-missed signs could lead to early intervention and better protection?
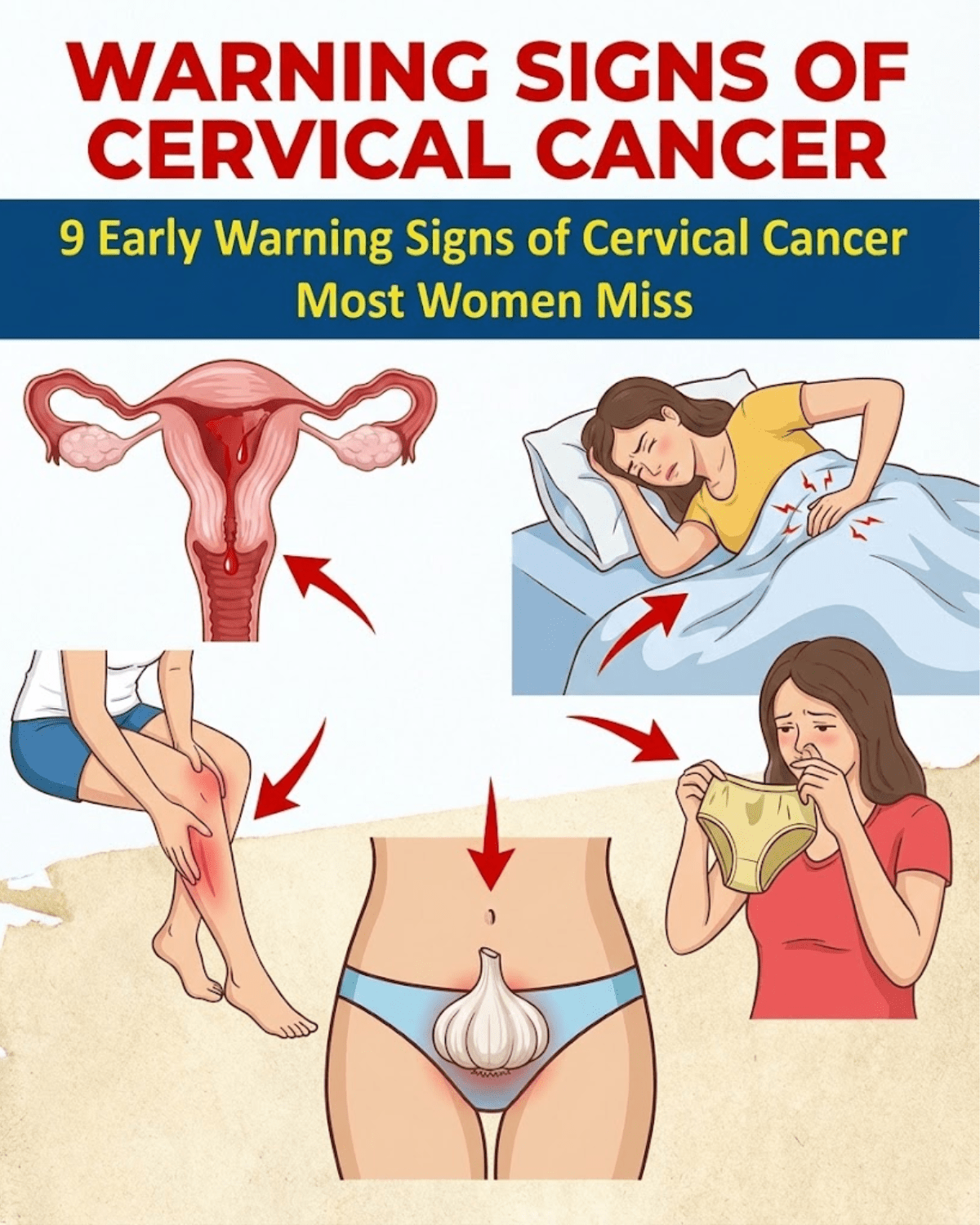
Stick around as we uncover 9 critical early warning signs of cervical cancer, real women’s journeys, and empowering steps forward. You’ll discover the science, stories, and simple actions that make a life-changing difference.
The Hidden Threat of Cervical Cancer—Why So Many Women Miss the Clues Until Later
Turning 35 often introduces unexpected shifts: busier schedules, hormonal fluctuations… and subtle body changes that get dismissed.
Data shows cervical cancer affects thousands annually, with many cases linked to persistent HPV infection—yet screening has reduced incidence by over 50% in past decades, though rates have stabilized recently.
It’s frustrating when vague symptoms like spotting disrupt your routine or intimacy feels off—sound familiar?
But it’s not just temporary inconvenience. Ignoring signs may allow progression, raising risks for advanced stages with tougher treatments and lower survival odds.
Have you paused to reflect on any recent pelvic or menstrual changes on a scale of 1-5? Be honest—what’s your score?
You’ve probably relied on routine checkups or ignored mild issues—often because early cervical cancer shows few obvious signals, delaying crucial action.
But what if tuning into your body early could shift everything? The insights start unfolding…
You’re in the top 40% of dedicated readers—keep reading for empowerment most overlook.
Why Early Signs Are Often Subtle Yet Critical—And How HPV Plays a Role
Ever had that nagging doubt about a symptom—like bleeding after intimacy—and pushed it aside thinking “it’s nothing”?
Picture this: You’re a dedicated mom or professional in your 40s, handling endless responsibilities, but persistent fatigue or discomfort creeps in unnoticed.
Quick self-check: On a scale of 1-10, how frequently do you notice unusual vaginal changes? If above 4, this could explain it.
Persistent high-risk HPV infection drives nearly all cases—often silent until changes appear.
For perfectionists prioritizing wellness, skeptics assuming “it’s rare,” or busy parents juggling life—this virus affects most sexually active people at some point, but persistent types raise concern.
I get it—you’ve dismissed changes before. You’re not overreacting; knowledge empowers timely steps.
Pause and think: What’s your biggest worry about reproductive health lately?
Sign 1: Abnormal Vaginal Bleeding That Feels “Off”
Unexpected spotting or heavier flows disrupting your cycle?
Meet Emily, 38, office manager from California. “Bleeding after sex scared me—dismissed it as rough intimacy at first,” she recalls.
Abnormal bleeding often signals changes in cervical tissue.
Guidelines highlight this as a key alert, especially post-intercourse or between periods.
Emily sought care promptly: “Early testing caught precancerous cells—treatment prevented progression!”
She felt relieved, proactive. “Doctor said, ‘You saved yourself years of worry.'”
Rate any unusual bleeding 1-10: If present, don’t delay.
But discharge changes next often go unnoticed…
Bonus tip: Track patterns in a health app—clues emerge.

Sign 2: Unusual Vaginal Discharge—Watery, Bloody, or Odorous
Sudden shift to foul-smelling or bloody discharge?
Sarah, 41, nurse: “Heavy, odd discharge embarrassed me—thought infection.”
May indicate tissue changes or infection.
Research links persistent unusual discharge to progression.
Sarah: “Testing revealed issues—early intervention restored normalcy.”
Emotional lift: From worried to confident.
Self-assessment: Rate discharge changes 1-10.
But pain during intimacy compounds anxiety…
Sign 3: Pain or Discomfort During Intercourse
Intimacy turning uncomfortable or painful?
Lisa, 39: “Sex became painful—avoided closeness, strained relationship.”
Tumor growth may cause friction or pressure.
Common yet underreported.
Lisa: “Addressed early—relief and intimacy returned.”
Quick exercise: Imagine comfortable, confident connection.
Only 6 signs left—stay engaged!

Sign 4: Pelvic Pain or Pressure That Lingers
Dull ache or heaviness in lower abdomen?
Rachel, 42: “Constant pelvic discomfort—chalked up to stress.”
May signal advancing changes pressing tissues.
Rachel: “Imaging and care eased it—peace returned.”
Rate pelvic discomfort 1-5.
You’ve unlocked key signs—top 30%!
Sign 5: Longer or Heavier Menstrual Periods
Cycles suddenly extended or intensified?
Anna, 37: “Periods dragged on—heavy bleeding exhausted me.”
Hormonal disruption from changes.
Anna: “Investigation caught early—managed effectively.”
Insider secret: Log cycles monthly—patterns matter.
Sign 6: Bleeding After Menopause
Any post-menopausal spotting alarming?
Karen, 52: “Thought menopause ended periods—spotting terrified.”
Classic red flag.
Karen: “Prompt check—early action prevented worse.”

Sign 7: Unexplained Fatigue or Weakness
Persistent tiredness beyond normal?
Tom’s wife, 45: “Exhausted constantly—brushed off as busy life.”
Systemic impact possible.
Supportive care helped.
Sign 8: Leg Pain or Swelling
Unusual lower limb discomfort?
May indicate advanced pressure.
Monitor closely.
Sign 9: Urinary or Bowel Changes
Frequent urges or difficulties?
Potential spread effects.
Pro strategy: Annual screenings essential.
You’re halfway—deeper empowerment ahead!
Bookmark for screening reminders.
Mid-Article Quiz Time! Deeper Engagement
- How many signs covered? (9)
- Biggest concern? (Note it)
- Predict next: Prevention?
- Rate awareness now vs start.
- Ready for more? (Yes!)
Fun, right? Onward…

Prevention and Early Action: Your Strongest Defense
HPV drives nearly all cases—vaccination prevents most.
Screening: Pap/HPV tests detect changes early.
| Sign | Common Dismissal | Why It Matters |
|---|---|---|
| Abnormal Bleeding | “Just irregular” | Often first alert |
| Unusual Discharge | “Infection” | May signal changes |
| Pain During Sex | “Temporary” | Tissue impact |
| Pelvic Pain | “Stress” | Possible progression |
| Age Group | Recommended Screening | Frequency |
|---|---|---|
| 21-29 | Pap test | Every 3 years |
| 30-65 | Pap + HPV or HPV alone | Every 3-5 years |
| 65+ | May stop if prior normal | Consult provider |
| Prevention Step | Benefit | Action Now |
|---|---|---|
| HPV Vaccine | Prevents most cases | Ages 9-45 |
| Quit Smoking | Lowers risk | Seek support |
| Safe Practices | Reduces HPV exposure | Consistent use |
Advanced Tips (Unlocked!):
- Discuss family history
- HPV self-testing options
- Maintain healthy weight
Welcome to 5% club!
Imagine 30 Days From Now…
Heightened awareness, prompt action on changes, peace from screenings. Feeling empowered, protected.
Inaction: Missed opportunities, advanced risks.
Reward: Early detection, higher survival, vibrant life.
Thousands prioritizing screenings—join them.
Schedule your next Pap or talk to your doctor today.
Every delay risks progression.
Share with women you care about.
You’ve unlocked all—top 1%!
Ultimate revelation: Prevention through vaccination and screening makes cervical cancer largely avoidable.
P.S. Final insider: Get vaccinated if eligible—protect yourself and others.
This article is for informational purposes only and does not replace professional medical advice. Consult your healthcare provider for personalized guidance, especially regarding symptoms or screening.