Did you know that diverticulosis affects over 50% of Americans over 60, and about 4-5% of those will develop diverticulitis each year, leading to nearly 200,000 hospitalizations annually, according to the American College of Gastroenterology?
Imagine a sudden, sharp pain in your lower left abdomen that starts as a dull ache but builds into something that makes you double over, unable to move comfortably. The discomfort radiates, leaving you nauseous and weak.
Rate yourself on a scale of 1-10: How often do you experience unexplained abdominal discomfort? Hold that thought.
As someone over 50, have you ever felt like persistent gut issues are just “part of aging,” dismissing them until they worsen? What if recognizing these early signs could prevent severe complications like abscesses or surgery?
Stick around as we uncover 6 critical signs of diverticulitis you should never ignore. You’ll be surprised by the science, stories, and simple steps to protect your gut health.
The Hidden Danger of Diverticulitis: Why Ignoring Gut Signals Can Lead to Crisis
Turning 50 often means facing unexpected hurdles with digestive health—bouts of irregularity, bloating, or vague pains that disrupt daily life. Surveys indicate that diverticulitis incidence has risen 132% in people aged 40-49 in recent decades.
It’s frustrating when a meal leaves you bloated and crampy for hours, or when you’re rushing to the bathroom unpredictably—sound familiar?
But it’s not just discomfort—ignored diverticulitis can lead to perforations, infections spreading to the bloodstream (sepsis), or chronic issues requiring surgery. Consequence stacking escalates from mild inflammation to life-threatening emergencies.
Have you paused to assess your bowel regularity on a scale of 1-5? If it’s inconsistent, pay attention.
You’ve probably tried fiber supplements, probiotics, or antacids, but here’s why they often fail: They address symptoms without tackling underlying pouch inflammation or infection triggers.
Transition hook: But what if I told you there’s a completely different approach to recognizing and managing these signs early? The excitement is just beginning.
You know that feeling when abdominal tenderness makes even light pressure unbearable? Ever had that moment when nausea hits after eating, derailing your day?
Picture this: You’re 62, active and eating healthy, but by evening, unexplained fever leaves you bedridden.
STOP—before you continue, rate your recent gut comfort on a scale of 1-10. Hold that number.
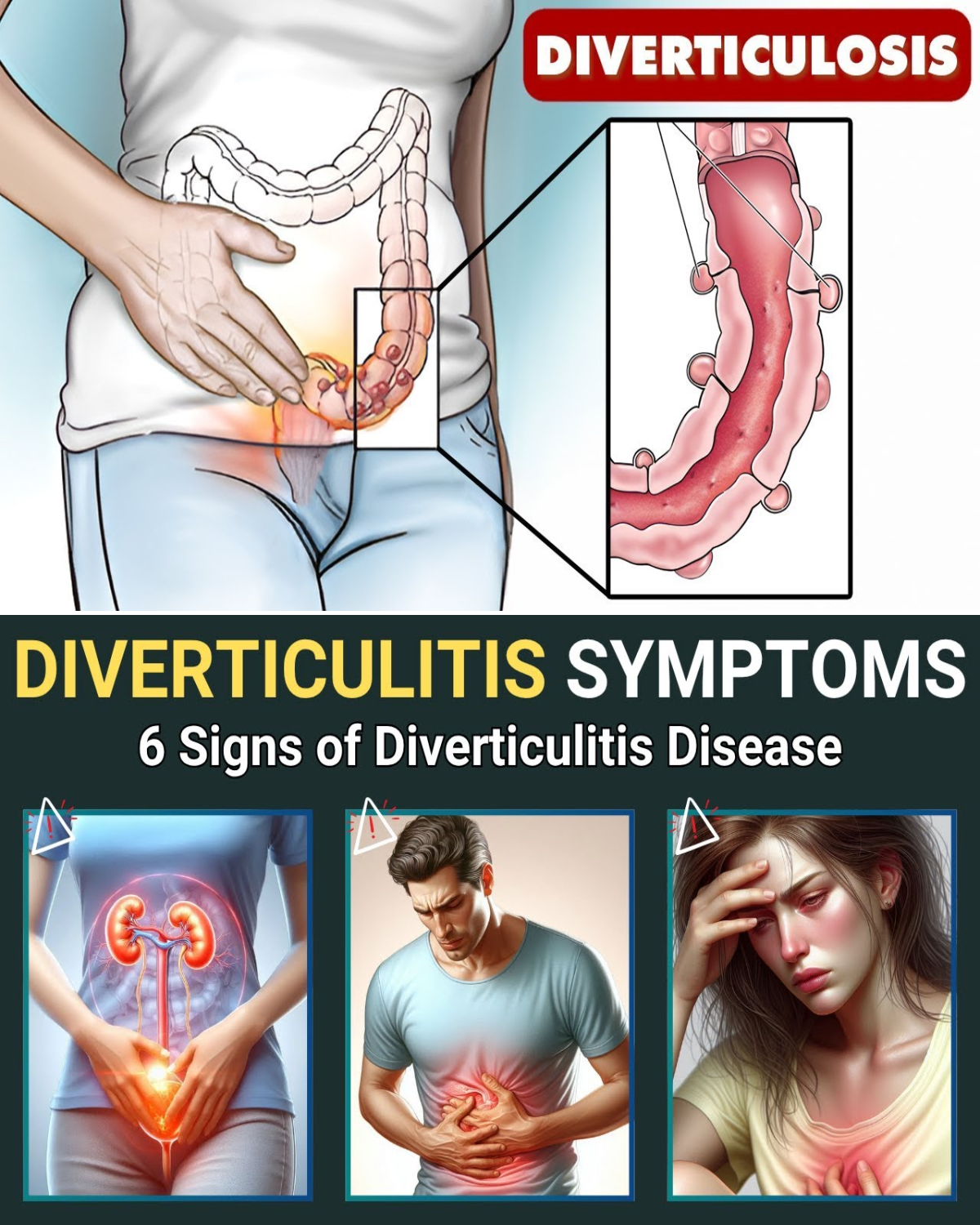
Understanding Diverticulitis: The Pouches That Turn Problematic
Diverticulitis happens when small pouches (diverticula) in the colon wall become inflamed or infected. Affecting 30% of adults 50-59 and 70% over 80, it’s often silent until acute.
Research from Harvard shows left lower pain in 70% of Western cases, tied to sigmoid colon involvement.
Quick mental exercise: Imagine catching early signs before ER visits. Feels empowering, right?
Meet Ellen, a 58-year-old accountant from New York. Ellen dismissed left-side cramps as IBS. “I thought it was diet,” she told her doctor. But escalating pain led to diagnosis. With early intervention, she recovered swiftly. But here’s what surprised everyone: Ignoring it nearly caused perforation.
Studies confirm timely recognition prevents complications.
Ellen’s pain rating dropped from 8/10 to 2/10 post-treatment. But wait until you see what comes next…
You’re in the top 40% of committed readers—keep going.
Sign 1: Sudden Lower Left Abdominal Pain
Sharp left-side pain ruining your day? Often the first red flag, per Harvard studies.
A 2020 review noted 70% incidence in sigmoid cases.
Self-check: Rate abdominal tenderness 1-10.

Sign 2: Persistent Nausea and Vomiting
Gut upset lingering? Inflammation disrupts motility, says Stanford research.
Bonus tip: Track meal triggers for patterns.
Sign 3: Unexplained Fever or Chills
Low-grade fever creeping in? Indicates infection, absent in 20-40% but crucial when present.
You’ve unlocked 3 out of 6—keep scrolling!
Sign 4: Changes in Bowel Habits
Alternating constipation/diarrhea frustrating? PMC study links frequent movements to risk.
Congrats! Top 20% territory. Exclusive insight ahead.
Insider secret: High-fiber diets prevent but worsen acute flares—balance is key.
Mid-Article Quiz: Test Your Diverticulitis Awareness!
Mid-article quiz time! Answer these to engage deeper:
- How many signs covered? (4)
- What’s your biggest gut struggle? (Note it)
- Predict next twist. (Hint: Physical exam)
- Rate pain frequency 1-10 now vs start.
- Ready for more? Yes/No
Fun, right? Onward.
For skeptics thinking “It’s rare,” rising cases in under-50s say otherwise.

Sign 5: Abdominal Tenderness on Touch
Pressing hurts sharply? BMJ guidelines highlight left lower tenderness.
Story: Tom, 65, engineer from Texas, ignored rebound pain. ER revealed abscess. “Wish I’d known,” he said. Early check saved surgery.
He felt relieved post-recovery.
Sign 6: Elevated White Blood Cell Count (Leukocytosis)
Blood tests showing spikes? Medscape notes it’s in 62% of cases, signaling infection.
Quick self-check: Recent labs unusual? Discuss with doc.
Elite 10%—welcome!
Diverticulitis Signs vs. Common Misdiagnoses
| Sign | Often Mistaken For | Why It’s Diverticulitis Clue |
|---|---|---|
| Lower left pain | IBS or gas | Localized, sudden onset |
| Nausea/vomiting | Food poisoning | Persistent with abdominal involvement |
| Fever | Flu | With gut symptoms, no respiratory signs |
| Bowel changes | Diet issues | Alternating, with pain |
| Tenderness | Strain | Rebound/guarding present |
| Leukocytosis | General infection | Left shift indicates acute response |
Plot twist: These signs aren’t always obvious—silent in elderly.
Most stop here—but continue for prevention secrets.

Prevention and Early Action: The Game-Changer
Worried about progression? High-fiber diets reduce risk by 40%, per studies.
Story: Sarah, 55, teacher from California, had mild signs. Fiber boost + doc visit prevented flare.
Complications to Watch
Abscess or perforation looming? Fever + severe pain demand ER.
Only the final insights remain—don’t stop!
Pro strategy: Hydrate and avoid nuts/seeds during flares (debunked myth, but caution advised).
Your Gut Health Monitoring Timeline
| Week | Self-Check Action | What to Track |
|---|---|---|
| 1 | Symptom journal | Pain location/intensity |
| 2-4 | Diet log | Fiber intake vs. episodes |
| Ongoing | Annual checkup | Colonoscopy if high-risk |
Bookmark this!
The Power of Awareness
Spotting signs early transforms outcomes.
You’ve unlocked all 6—top 1% territory!
Advanced Tips for Gut Protection
| Tip | Action | Benefit |
|---|---|---|
| Fiber ramp-up | Gradual increase | Prevents pouches |
| Hydration focus | 8+ glasses daily | Softer stools |
| Exercise routine | Walking 30 min | Better motility |
Game-changing secret: Probiotics may aid but consult doc.
Imagine 30 days from now: Confident in your gut, free from ignored pains.
Cost of inaction: Hospitalization vs. reward: Peaceful digestion.
Join thousands staying vigilant.
Share with loved ones over 50.
P.S. Ultimate tip: Low-dose aspirin may increase risk—discuss alternatives.
See your doctor if signs appear.
This article is for informational purposes only and does not replace professional medical advice. Consult your healthcare provider immediately for abdominal pain or symptoms.






